Abstract
Introduction
Transplant outcomes for TP53+ AML have been poor and survival is arguably one of the worst in transplantation. Here we hypothesized that outcomes of TP53+AML/MDS patients are not uniformly poor and aimed to identify prognostic factors for survival for patients with TP53+ AML receiving allogeneic hematopoietic stem cell transplantation.
Methods
A total of 83 patients with AML, MDS or MDS progressed to AML treated between 02/2011-03/2017 who received their first allogeneic transplant were identified in the departmental database. The median age was 60 years (range 18-75), median hematopoietic stem-cell transplantation - comorbidity index (HCT-CI) was 4 (range 0-9), Karnofsky performance status (KPS) was >80% (56%). 31 patients (37%) were in CR1/2 the rest were beyond CR1/2. Conditioning regimens were busulfan-based (83%) for HLA-matched transplants and melphalan-based (16%) for HLA mismatched transplants. Donors were matched related (33%), matched unrelated (49%), haploidentical (14%), cord blood (CB) (2%). 39% of the patients had a bone marrow graft while 59% had peripheral blood graft, 2% of the patients had a CB graft. 87% of AML patients were de novo and 13% treatment-related, and 13% of AML/MDS were secondary. Cytogenetic risk group was poor-risk in 99% of the patients. Eleven patients (13%) received maintenance azacitidine post-transplant.
Results
The median follow-up survivors was 12 months (2.2-42 months). Twenty-one patients (25.3%) were alive at last follow-up and 14 patients (16.9%) disease-free. The median overall survival (OS) was 8 months with 1-year OS 35% (range 25-46%), median progression-free survival (PFS) was 5 months with 1-year PFS 25% (range 16-35%). Non-relapse mortality (NRM) and relapse at 1 year were 20% and 53%, respectively. We evaluated predictors for NRM, relapse, PFS and OS considering the following variables: age, HCT-CI>4 vs. ≤4, KPS >80% vs. ≤80%, disease status CR1/2 vs. other, conditioning regimen, cell source, secondary AML/MDS (Y/N), treatment-related AML/MDS (Y/N) and azacitidine maintenance as a time-dependent variable. In univariate analysis (UVA), factors associated with NRM were HCT-CI>4 (HR2.8,CI1.1-7.6,p=0.04), melphalan-based regimen (HR 4.2,CI1.5-12,p=0.01), KPS≤80% (HR2.6,CI0.9-7.5,p=0.08) and treatment-related AML/MDS (HR3.3,CI1.2-9,p=0.02), while in multivariate analysis (MVA) factors associated with NRM were melphalan-regimen (HR6.5,CI2.1-20,p=0.001), KPS≤80% (HR2.8,CI0.96-8,p=0.06) and treatment-related AML/MDS (HR4.2,CI1.5-12,p=0.007).
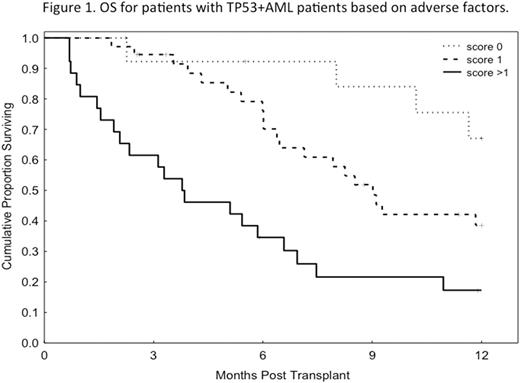
In MVA, factors associated with better PFS were KPS>80% (HR2.1,CI1.1-3.7,p=0.02) and mid-range busulfan-based conditioning with AUC 20,000-25,000 (HR1.7,CI0.96-3.0,p=0.07), while factors associated with worse OS were HCT-CI>4 (HR3.9,CI1.2-13,p=0.03), KPS≤80% (HR3.04,CI1.6-5.9,p=0.001) and disease not in CR1/2 (HR4.1,CI1.5-11,p=0.004). Since the HR were comparable for the 3 factors, we assigned a score of 1 for each factor and evaluated OS based on the number of adverse prognostic factors present. If none of these factors were present the 1-year OS was 67% (N=14; HR0.2,CI0.05-0.5,p=0.001), if 1 factor was present the 1-year OS was 39% (N=36; HR0.4,CI0.2-0.7,p=0.002) if >1 factor was present the 1-year OS 17% (N=27) (reference) (Figure 1). Azacitidine maintenance did not impact OS or PFS in these patients.
In conclusion, patients with TP53+AML can be stratified based on performance status, comorbidity index and disease status at transplant with significant impact on survival. Unfortunately two thirds of all patients were transplanted beyond CR1/2, which could be a contributing factor for the overall poor outcomes in these patients.
Khouri: Novartis: Research Funding.
Author notes
Asterisk with author names denotes non-ASH members.